It would be unwise to put it mildly.
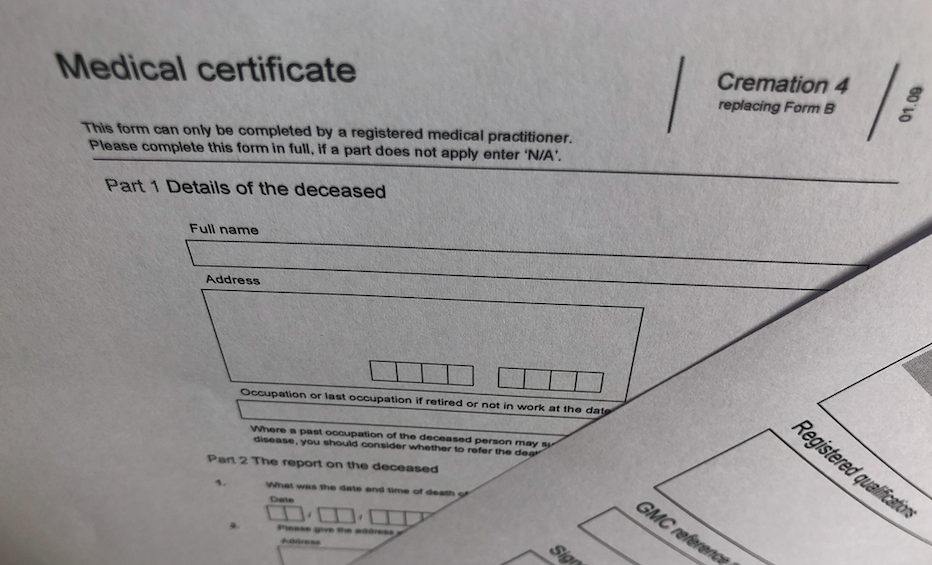
A funeral parlour director contacted Dr D to sign a Form 5 and impressed upon him that there was a degree of urgency relating to the form being signed. The deceased’s usual doctor was away and the family were becoming distressed about the fact that there was a delay. As most practitioners, and certainly GP’s will be aware, the process for certifying cremation certificates changed in 2022. At the time of Dr D’s signing Form 5 however, the procedure was that a doctor ticked a box to confirm that they had spoken with the deceased’s doctor who signed Form 4 and this verified that Form 4 was correct.
Dr D ticked the box stating he had spoken to the deceased doctor when in fact he had not. He telephoned the deceased’s doctor and was told only that she was ‘unavailable’. He was not told that she was on holiday. Dr D explained that he fully expected the doctor to phone him back, they usually did so within minutes. At the MPTS hearing he also gave evidence that he had spoken to a relative of the deceased and examined the body. His motivation was to alleviate some of the distress to the relatives so preparation of the body could begin, there was no financial motive. The GMC’s case was that Dr D was dishonest. This was rejected by the Tribunal. Dr D’s intentions were kind, it was a picosecond decision, he was busy at the time and he had never ticked the ‘no’ box before. It was a couple of days later that it occurred to him that he had not spoken with the Form 4 doctor and he then made contact.
The GMC took the view that circumventing the safeguards in cremation procedure was serious, Doctor D admitted that it was misconduct and the Tribunal also determined it was serious misconduct. On the facts however the Tribunal declined to find Dr D’s fitness to practise was impaired. There was a wealth of remediation experience and insight together with a low likelihood of any repetition. The Tribunal did issue a warning, they took the view the act was an act of convenience over propriety and a third party may have been misled.
Paragraph 19 of GMP states that “Documents you make (including clinical records) to formally record your work must be clear, accurate and legible. You should make records at the same time as the events you are recording or as soon as possible afterwards.”.
It is also worth pointing out that Dr D was far from inexperienced having been a GP for more than 30 years. He held a spotless record and glowing testimonials about his work were beneficial evidence sparing him more serious consequences.